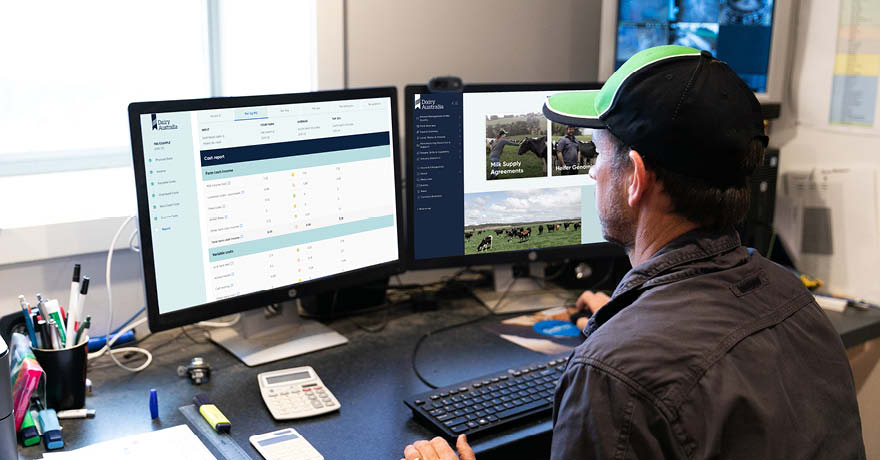
Dairy Australia provides farmers with access to business plans, risk management tools and insights that support decision making and improving profitability.
Information and resources below will support dairy farmers in business fundamentals, planning and risk, and budgeting and analysis.
Dairy Australia works across all regions to build farm business capability and equip farmers to make better decisions that increase profit and wealth over time. We want farmers to achieve their long term business and personal goals.
Our Farm, Our Plan
Our Farm, Our Plan helps farmers identify long term goals, improve business performance and manage …